Rosacea is common, and it’s also complicated to manage. Many more than 16 million Americans have rosacea—and most don’t know it, according to the National Rosacea Society. Identifying classic rosacea is easy, but identifying the more subtle forms is not; yet these will be some of your trickiest and most sensitive skin clients. Give them the wrong treatment or advice, and you can exacerbate their rosacea, potentially causing hyperpigmentation, scarring and a very unhappy client. Give them the right advice, and you have a loyal client and big fan who will help build your business.
As a skin care professional, you need to be familiar with all the types of rosacea. This article will help you better understand rosacea and will teach you how to identify some of the more subtle signs. Guidelines for choosing the right treatments will be provided, as well as tips to help you identify when your client needs to see a dermatologist for prescription treatments.
What is rosacea?
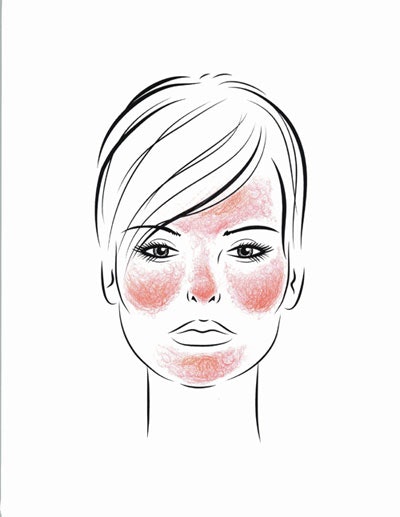
Rosacea is a rash of adulthood. Any adult is at risk, but rosacea is most commonly seen in light-skinned women between the ages of 30–50. It is characterized by persistent redness of the rounded areas of the face, including the cheeks, nose, chin and mid-forehead. It often spares the skin around the eyes. (See Facial Distribution of Rosacea.)
The skin looks red, hot and inflamed, but it is not infected. Rosacea is an inflammatory condition, and the location and pattern of the inflammation determines the type of rosacea it is.
1. Erythematotelangiectatic rosacea. This is the subtype in which inflammation is more diffuse in the skin, and is associated with redness and flushing. It may be dramatic or it may be quite subtle. With this type:
- There is often a history of flushing episodes lasting more than 10 minutes and occurring due to various stimuli, including emotional stress, hot drinks, alcohol, spicy foods, exercise, cold or hot weather, and hot baths or showers;
- The skin may sting or burn with flushing; and
- The skin is often finely textured with scaling and roughness of the central face—this is a big tip-off that your clients’ skin is sensitive. They will probably tell you that their skin is easily irritated, so you need to ask them about past product and treatment sensitivities.
2. Papulopustular rosacea.This is the classic rosacea subtype, with skin inflammation heavily centered around the pore, causing pimplelike redness and swelling, sometimes with pustules and nodules.
- There is often a history of flushing.
- There may or may not be a history of sensitive skin.
- The skin may be sebaceous and oily, red, thick and swollen.
3. Glandular rosacea with or without rhynophyma. This is a deep sebaceous rosacea subtype, most commonly seen in men with a history of teenage acne. With this type:
- Flushing and telangiectasias are less prominent;
- Skin is thick and sebaceous, and it is not sensitive or easily irritated;
- Pores are large and filled with plugs of dead skin cells and sebum; and
- There is swelling and enlargement of the oil glands that is classically evidenced by a larger, rounded nose.
4. Ocular rosacea. This is inflammation of the oil glands along the eyelash line and can be seen with all the types of rosacea.
- Some studies have linked it to demodex mites.
- There can be redness, irritation and grittiness of the eyes, stinging, burning and light sensitivity.
- Ocular rosacea may precede facial skin involvement.
Why do people get rosacea?
No one knows! What is known includes the following.
1. The regulation of blood flow to the skin in rosacea is abnormal. People with rosacea have an abnormal vasomotor response of their facial capillaries to heat and other flushing stimuli, leading to easy and frequent flushing.
2. Demodex mites have been implicated in some studies. However, the role of demodex mites remains controversial. A recent study suggests that a protein on a bacteria on the mites might be important, but it’s a to-be-continued story because:
- Pores with demodex mites are more likely to be inflamed; however, 100% of elderly people have demodex in their pores and not all have rosacea;
- The presence of demodex mites is most closely associated with inflammatory papulopustular rosacea; and
- Killing the demodex mites with medicine does not necessarily cure rosacea.
3. Intestinal bacteria, such as Helicobacter pylori, have been implicated as well, but there is evidence both for and against this hypothesis. It may turn out that it’s more important for some people than others.
Identifying rosacea
Classic rosacea is easy to identify, but subtle rosacea can be tricky. The three most common conditions that may mimic rosacea include:
- Non-rosacea forms of acne;
- Skin rashes of allergic and irritant dermatitis; and
- Facial dandruff (seborrheic dermatitis).
Tips to tell acne from rosacea.
- Look for blackheads, not just engorged and clogged pores—blackheads are more common in acne.
- How old is your client? Acne is more common in adolescents and young adults.
- Female hormonal acne happens in adulthood, but it usually manifests as big, painful cysts along the jaw, which is not a common site for rosacea.
Tips to tell rosacea from the red and scaly rashes of dermatitis and dandruff.
- Is the condition caused by a potential product allergy or irritation? Check and see if the irritation is located only where a product is being applied.
- There is often an itching with allergic reactions. Poison oak or ivy is a classic example of allergic dermatitis. Many ingredients in skin care products can be allergens, too.
- There is often a dry, chapped appearance with stinging in irritant reactions. Classic examples are alpha hydroxy acid (AHA) or acne products that are too strong for a client.
- Dandruff usually involves the eyebrows, hairline, ears and along the sides of the nose more than the convex surfaces of the face. (See Facial Distribution of Seborrheic Dermatitis.)
- Dandruff often occurs with rosacea, and the good news is that the treatments overlap.
Part II
In Part II of this article, which will appear in the August issue of Skin Inc., in-depth information will be provided about how to design a skin care program for clients with rosacea. A class will also be offered on this topic by Cynthia Bailey, MD, at Face & Body® Northern California in San Jose on August 24, 2013, during the Advanced Education Conference Program. To register, log on to www.FaceandBody.com/california/register!
GENERAL REFERENCES
HE Baldwin, Diagnosis and treatment of rosacea: state of the art, J Drugs Dermatol 11 725–730 (2012)
AW Borkowski and RL Gallo, The coordinated response of the physical and antimicrobial peptide barriers of the skin, J Invest Dermatol 131 285–287 (2011)
JQ Del Rosso, et al., Why is rosacea considered to be an inflammatory disorder? The primary
role, clinical relevance, and therapeutic correlations of abnormal innate immune response in rosacea-prone skin, J Drugs Dermatol 11 694–700 (2012)
DM Elston, Demodex mites: facts and controversies, Clin Dermatol 28 502–504 (2010)
F Forton and B Seys, Density of Demodex folliculorum in rosacea: a case-control study
using standardized skin-surface biopsy, Br J Dermatol 128 650–659 (1993)
YY Gao, et al,. In vitro and in vivo killing of ocular Demodex by tea tree oil, Br J Ophthalmol 89 1468–1473 (2005)
WD James, T Berger, GV Elston, DM Andrews, Diseases of the Skin: Clinical Dermatology, 11th Edition, Elsevier Inc., Philadelphia, 241–244 (2011)
S Jarmuda, et al., The potential role of Demodex folliculorum mites and bacteria in the inductio of rosacea, J Med Microbiol 61 1504–1510 (2012)
J Li, et al., Correlation between ocular Demodex infestation and serum immunoreactivity to Bacillus proteins in patients with facial rosacea. Ophthalmology, 117 870–877 (2010)
S Utaş, et al., Helicobacter pylori eradication treatment reduces the severity of rosacea, J Am Acad Dermatol 40 433–435 (1999)
RT Vollmer, Demodex-associated folliculitis, Am J Dermatopathol 18 589–591 (1996)
YE Zhao, et al., Retrospective analysis of the association between Demodex infestation and rosacea, Arch Dermatol 146 896–902 (2010)