The anti-aging market has long been considered a booming business, and the past few years have seen a notable shift in how aging is viewed. The hot topic is the distribution of melanin, or pigmentation, in skin as a marker of age.
Of course, fine lines and wrinkles are the old standbys of anti-aging vocabulary, and they continue to be of concern to clients worldwide. However, current consumer research indicates that uneven skin coloring—specifically, the blotches and dark spots on the face, décolleté and hands, which is a classic indicator of UV exposure and hormonal shifts—now matches or even surpasses concerns about skin smoothness and texture.
Do ask, do tell
As a skin care professional, use your skills to address pigmentation in the context it deserves: as a factual part of the client’s scientific and chemical composition. Knowing ancestry detail will be ideal information when developing a treatment plan.
The color of skin as an innate aspect of physiology is hereditary. With modern society being an increasingly rich mix of ethnicities, observation alone does not tell you enough. Treating changes in pigmentation is about becoming a bit of a DNA sleuth. Asking key questions will help. During the consultation, take the time to identify clients’ ethnic heritage as specifically as possible:
- Find out how their skin responds to sun exposure;
- Question genetics past examining hair color and color of skin; and
- Ask about their habits regarding sun exposure.
Appearances can often be deceiving; especially as the years pass, sun exposure and other environmental factors may alter the superficial appearance of the skin. When working with pigmentation, there are always underlying components that may counter-indicate specific treatment.
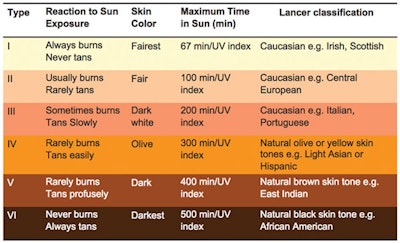
For example, someone with visibly light skin may possess ancestry that counter-indicates chemical peels or other aggressive procedures. To get a baseline reading, incorporate a combination of the Fitzpatrick Skin Type Classification Scale for inflammation response and the Lancer Ethnicity Scale for ethnic heritage into skin care consultations. (See Combined Fitzpatrick & Lancer Ethnicity Scale.)
Common hyperpigmentation issues
Analyzing pigmentation is a nuanced aspect of the skin care profession. Begin by familiarizing yourself with these common pigmentation issues, and remember that the client may have several simultaneous conditions.
Drug-induced hyperpigmenation (DIH). Although not considered a main factor, changes in pigmentation are usually due to illnesses, certain prescription medications or reactions of the drug. DIH, when observed, takes on a more diffused look. Specific patterns or hues have been observed. See Shades of Drug-induced Hyperpigmentation sidebar.
Lentigines. Commonly known as liver spots or age spots, lentigines are benign pigmented spots with a clearly defined edge. While not directly caused by the aging process, they become more prevalent with age. Related to UV exposure, lentigines are found on 90% of light-skinned individuals over the age of 60. However, they will stay stable in color regardless of sunlight exposure, unlike freckles.
Melasma. Caused by hormonal fluctuations, melasma is common, for example, during pregnancy, with some thyroid dysfunctions, and through use of birth control pills and hormone replacement therapy. One of the most challenging pigmentary conditions to treat, melasma affects more than five million Americans.1 It normally appears on sun-exposed areas of the face and as flat distinct areas of discoloration.
Phytophotodermatitis. A phototoxic chemical reaction that results from sensitivity to ultraviolet light, phytophotodermatitis is caused by contact with the photosensitizing compounds, specifically furocoumarins found in some plants and vegetables, such as limes, parsley and celery.
Post-inflammatory hyperpigmentation (PIH). PIH occurs following an injury, such as burns, friction, and even professional skin treatments, including extractions and chemical peels, or from other causes of inflammation such as acne. Traditionally, PIH will resolve and fade over time as the skin regenerates itself, but this could take months. PIH is normally the easiest type of hyperpigmentation to treat and generally responds well to treatment.
Choosing ingredients and products
Knowing as much as possible about clients means that you will be best-equipped to create a treatment that is safe, as well as successful. It is an irony that deeply pigmented skin often seems to age more gracefully than fair skin—but darker skin is prone to forming pigmentation reactions, including PIH or even raised scarring, such as keloids. A common example of PIH is the formation of darkened razor bumps, or pseudofolliculitis, along the beard-line in men with deeply pigmented skin.
When designing a brightening treatment, the level of exfoliation in particular must be carefully aligned with the tolerance and anticipated reactiveness of the client’s skin. For the most effective desquamation with the lowest incidence of trauma, treatments with papaya enzyme (papain), pumpkin enzyme, lactic acid and sugar cane extract are recommended for all skin types. Salicylic acid and trichloroacetic acid (TCA) also can be used to increase cell turnover, but are more aggressive than the former. Proper education and training should be exercised before performing more advanced treatments.
With the long-term health of the client’s skin in mind, select leave-on products that feature and sometimes combine the following ingredients.
Glucosamine. A favorite of cosmetic formulators, glucosamine interrupts the UV-triggered chemical signals that turn on melanin production.
Hydrolyzed pearl powder. This ingredient increases luminosity to the skin and inhibits tyrosinase.
Licorice root extract (Glycyrrhiza glabra). A Licorice root extract is an antioxidant that scavenges free radicals, inhibits oxidation, and inhibits tyronsinase synthesis and activity.
Niacinamide (vitamin B3). Niacinamide prevents the transfer of melanosomes to keratinocytes, minimizing color deposits. Inflammatory mediators also are inhibited, reducing pigmentation associated with PIH.
Phytic acid. This ingredient chelates copper and inhibits melanogenesis.
Soy. A derivative from the soybean plant, soy inhibits the transfer of melanosomes and can also inhibit the signal from the keratinocyte.
Strelitzia nicolai seed extract. Also known as Giant White Bird of Paradise, Strelitzia nicolai increases skin luminosity while improving hydration and smoothness.
Vitamin C and its derivatives. Vitamin C is an antioxidant that scavenges free radicals, inhibits oxidation and tyronsinase synthesis and activity.
Zinc glycinate. This ingredient stimulates the formation of an antioxidant protein to bind copper and inhibit the production of melanin.
The latest agents to fight formation of hyperpigmentation are ground-breaking peptides.
Azelaic acid. A naturally occurring, non-toxic fatty acid developed for the treatment of acne, azelaic acid has proven to be beneficial in the treatment of hyperpigmentation, especially PIH from acne lesions. In one study, it demonstrated results similar to 4% hydroquinone, but without its side effects,2 though it may also have both cytotoxic and anti-proliferative effects on melanocytes.
Kojic acid. From the fungus Aspergilline oryzae, kojic acid is a tyrosinase inhibitor. Formulated alone or combined with hydroxy acids or other skin-lightening agents, it can be used as an alternative for those who may have a sensitivity to hydroquinone. The drawback is that it has the potential to cause contact dermatitis.
Oligopeptide-34. This ingredient reduces overall melanin formation and tyrosinase enzyme activity, and stands as a competitor to arbutin and vitamin C.
Oligopetide-51. A new proprietary peptide, oligopetide-51 inhibits melanin formation, tyrosinase activity and six different stages within melanin production.
Retinoids. Vitamin A or prescription tretinoin 0.05%–0.1% reduces pigmentation by inhibiting tyrosinase, as well as by interrupting melanin synthesis. While tretinoin may be effective in reducing pigmentation—especially melasma, it can typically take up to 24 weeks before seeing any clinical improvement. Prescription retinoids also may increase pigmentation secondary to irritation, resulting in cause erythema and peeling. Other retinoids or derivatives of vitamin A can be used that lessen the chance of irritation. Some of these ingredients are hydroxypinacolone retinoate, retinyl palmitate, retinol or retnoic acid.
Many topical therapies contain a combination of various ingredients including the above and sometimes corticosteroids to combat skin irritation.
Ingredient knowledge combined with a proper skin assessment will help identify the changes in hyperpigmentation, why it responds to stimuli in the manner that it does, and what professional skin care protocols are appropriate.
Managing expectations
When addressing hyperpigmentation concerns, it is essential to manage client expectations wisely. In an age of instant gratification and “overnight results,” clients may want a lifetime of sun damage or other pigmentation-related conditions undone as if by magic. Always proceed with caution, and take a conservative and patient approach. Speak candidly with your client, and explain that smaller steps will produce effective results with less risk of further damage.
REFERENCES