Evidence was found to suggest the makeup of the skin microbiome can affect the ability of a bacterial pathogen to cause an infection. The results help provide another example of how the ecology of human skin can influence health and disease.
The authors of these findings include Stanley Spinola, M.D., professor and chair, Department of Microbiology and Immunology, Indiana University and his colleagues, who used a system based on human volunteer inoculation for this study.
“This is an interesting report, and most important, because it takes yet another step toward seeking evidence of a clear function of the microbiome,” said Richard Gallo, chief of dermatology, University of California, San Diego, School of Medicine, who was not involved in the study.
Infection Model Testing
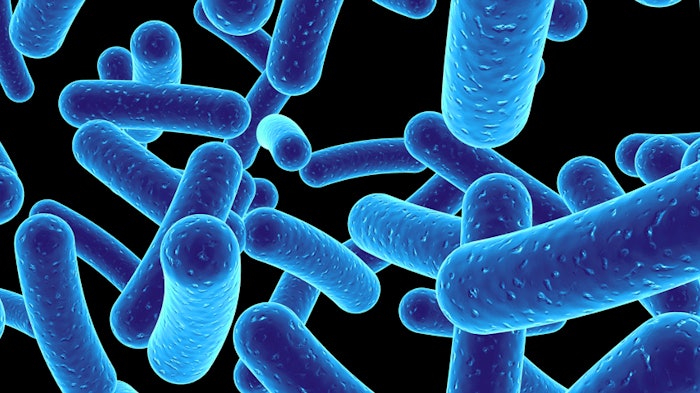
Previously, Spinola’s laboratory developed an infection model in humans of Haemophilus ducreyi, a bacterial species. This bacterial species causes chancroid, a common form of sexually transmitted genital ulcers endemic in certain parts of Africa and Asia. The bacterium was also implicated in chronic skin ulcers in children, seen in individuals in regions of equatorial Africa and the South Pacific islands.
H. ducreyi initially forms a red bump called a papule, which is cleared without any intervention in about 30% of tested volunteers. The remaining people go on to develop pustules, which if not treated, can form skin ulcers.
For the current study, researchers inoculated volunteers with a set dose of the bacteria on their upper arms and allowed the infection to progress up to several days to the pustule stage.
“We have one of few bacterial models in which you can actively infect people,” said Spinola. “And the reason we can ethically do this is that the [inoculation] just causes a local infection that we can terminate with antibiotics.”
Performing the Study
Prior to infecting eight individuals with H. ducreyi, researchers took skin microbiome samples during days one through five of infection in addition to the time of pustule formation or following infection resolution.
Four study participants resolved the infection on their own, while the other four progressed to the pustular infection stage. All of the participants were treated with antibiotics, no matter their infection outcome.
“It is uncommon to perform inoculation studies in research volunteers with bacteria that can cause infections, but studies like this one could provide valuable insights into the pathogenesis of diseases,” said Heidi Kong, who studies the skin microbiome at the dermatology branch of the Center for Cancer Research in Bethesda, Maryland.
Predicted Outcome
The researchers found the microbiome community structure—the species and their relative distribution—was similar among people who unexpectedly resolved their infections. In contrast, those four who developed pustules each had very different microbiome compositions. In people who progressed to an active infection, the microbiome was much more dynamic from the beginning of the experiment to the end.
“The pustule-formers started out with dispersed microbiomes that were then driven to a similar composition,” explained Spinola.
“The resident microbiota are antagonistic to invaders whether they are in the gastrointestinal tract or skin and they don't want to share their home turf,” said Martin Blaser, microbiologist of the New York University Langone Medical Center, who was not involved in the study.
Spinola’s team is planning follow-up studies on a larger group of individuals and to expand the microbiome analysis to also include the viral and fungal components of the skin. His team is also working on a preliminary study on the role of the genetics of the immune system in response to similar bacterial infections.