Rosacea is a chronic skin disorder characterized by microcirculation problems that primarily affect the face. It’s comprised of several related symptoms, such as couperose, or the dilation of facial blood vessels, and erythema, or redness. Extra-facial lesions on the neck and upper chest are not uncommon. The word “rosacea” comes from the Latin rosacea, derived from rosaceus meaning “pinklike.”
Approximately 16 million Americans and 45 million people worldwide suffer from rosacea. According to the National Rosacea Society (NRS), a Gallup survey found that 78% of Americans have no knowledge of this condition, including how to recognize it and what to do about it. (See Be Knowledgeable About Rosacea.) Although symptoms may occur during the teenage years, most people experience the onset of rosacea in their 30s, 40s or 50s, and it is more predominate in fair-skinned women. The precise cause of rosacea remains unknown, but research has shown that many factors are involved, such as genetic predisposition, heredity—especially European/Celtic descent, stomach dyspepsia and Helicobacter pylori infection, seborrhea, Demodex folliculorum mites, endocrine disorders, vitamin deficiency, liver disease and stress-related causes.
Discerning the enigma
Rosacea clients are generally prone to flushing and blushing mainly on the t-zone and cheeks. This can occur either spontaneously or can be precipitated by certain triggers that play a particular role in the development of this skin disorder, including the following.
- Emotional stress
- Heat and abrupt temperature changes
- Caffeine
- Sunlight and repeated sunburning
- Alcoholic beverages
- Spicy foods
- Foods that contain histamine or cause the body to release histamine, such as tomatoes and pineapples
- Medications, such as steroids
For example, a rosacea client may experience facial redness after drinking a hot beverage. One possible explanation would be that the heat from the beverage warms the blood irrigating the pharynx, which causes redirection of the blood flowing to the face from the brain, creating unwanted congestion at the facial level.
According to scientific belief, blood vessels become damaged when they are repeatedly dilated by stimuli, in part mediated by the hypothalamus. It has been proposed that the local release of vasoactive substances has an important implication in this pathology causing inflammation, stagnation and congestion of blood. Associated factors include minor vascular anatomical disorders, and dysfunction of the thermoregulatory vascular cooling system of the brain. These factors are partly responsible for causing blood backflow to the face with increased vessel pressure that secondarily affects the subpapillary venous plexus, leading ultimately to permanent vasodilation. Other very important factors that play a major role in damaging blood vessels include deterioration of the dermal matrix and the atrophy of supporting vessel tissues.
Also, pertaining to this disease and the role of microorganisms, greater numbers of D. folliculorum mites—part of the skin’s normal flora—are found in some rosacea clients who exhibit papulopustular eruptions. One theory proposes that changes in connective and vascular tissue provide a favorable environment for the mites to multiply. Potentially, the mites can cause an immunologic reaction that triggers an inflammatory response. This contributes to the aggravation of the symptoms.
Furthermore, it has been suggested that H. pylori,an ulcer-related agent, synthesizes gastrin in the stomach, which has been linked to promoting flushing. The participation of microorganisms in the development of this disorder continues to remain unclear at this time, as study results are inconclusive and inconsistent. Further research is necessary.
Evolution of the disease
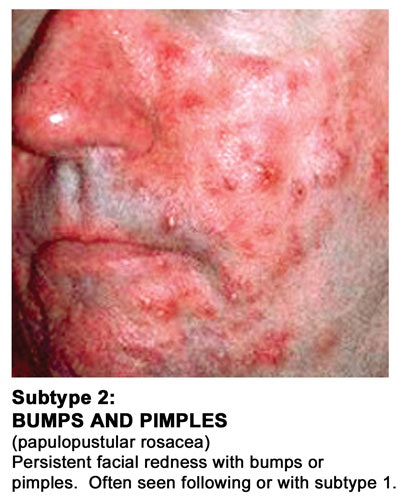
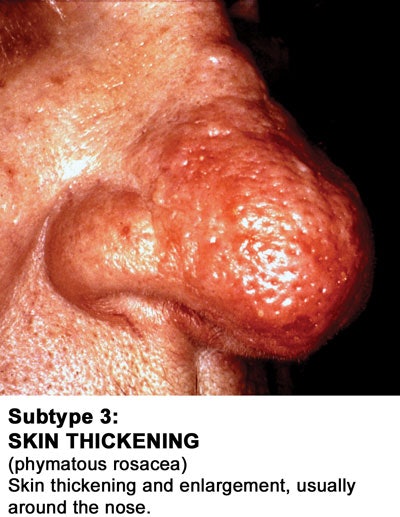
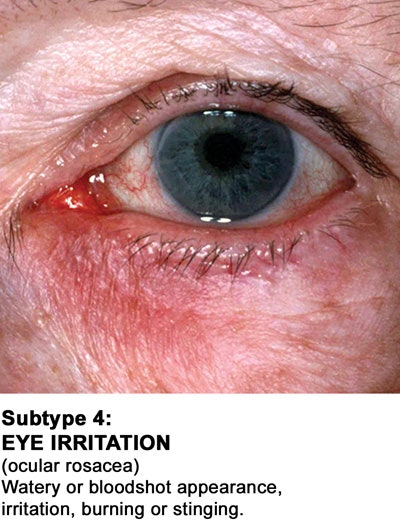
The evolution of rosacea affecting the skin usually progresses from a mild stage, including redness and increased skin sensitivity, to a later stage, including papulopustular eruptions, commonly known as acne rosacea. As the condition evolves, it may present complications such as rhinophyma, a nose enlargement mostly affecting men, and rosacea fulminans, featuring pyoderma faciale abscesses and nodules. Fortunately, fulminans is a rare complication. Advanced and chronic schemes of the disease may additionally present sebaceous hyperplasias, fibrosis and lymphedema, or swelling. Ocular rosacea may be accompanied by inflammation inside the eyes, lids and surrounding area. In some cases, recurrent conjunctivitis and periorbital lymphedema are reasons why people consult their physicians.
The causative reasons for acne and acne rosacea are different. Acne originates primarily within the hair follicles and does not involve microcirculation; a very inflamed acne, though, can resemble rosacea, which results in the confusion. Acne rosacea, identified by inflamed and raised lesions over an erythematous area, develops as papules and pustules that may foster parasitic microorganisms. Unlike common acne breakouts, the problem is not from bacteria, retention hyperkeratosis (dead cell retention) and excess sebum, but from a combination of parasitic activity and tissue inflammation. Clients may or may not report oiliness of the skin; sometimes they may actually experience drying and peeling. For skin care professionals, the most interesting and easily recognizable features of acne rosacea versus acne are the absence of comedones and minimal scarring in the former, plus a logical correlation with the history of the condition, which can be identified during consultation.
Last but not least, there is also neck rosacea, which appears as a dilation of capillaries with diffused v-shaped reddish-brown discoloration on the sides of the neck, and a gooseflesh appearance of the skin. This occurs due to repeated exposure to sunlight or sunburn on rosacea-prone skin, causing partial atrophy of the epidermis and dermis, but sparing the tissue surrounding the hair follicles, therefore creating a bumpy look and feel.
Treating rosacea
At the moment, there is no complete cure for rosacea, but it can be greatly improved with treatment. Early stages of the disease are characterized by minor cosmetic disabilities. The good news is that not everyone affected will develop every stage of the disease. It is imperative that control and action are taken to avoid further deterioration of both the condition and the person’s wellness.
Rosacea demands skin care. Proper treatment of the skin is vital to improve the symptoms and enhance the client’s quality of life. There are many courses to addressing rosacea from a medical standpoint, as well as from the esthetic approach.
Current medical treatments, for the most part, are effective in controlling symptoms associated with D. folliculorum mites and prevalence of redness. Physicians usually agree on treating rosacea by combining topical and systemic therapies. Some topical agents have proven somewhat effective in suppressing flares and producing a reduction in the parasitic infestation, including, but not limited to, metronidazol and sulfacetamide. Popular systemic agents include tetracyclin and minocycline. As with most prescription therapies, side effects may be unavoidable, especially if the drugs are utilized long-term.
Laser and intense pulsed light (IPL) have shown remarkable results to improve facial flushing and erythema by targeting dilated blood vessels causing their atrophy and removal. LED light therapy has also proven somewhat beneficial for rosacea, especially when it comes to gentle healing and decreasing inflammation.
For the skin care specialist in the field of esthetics, there are ready-to-use alternatives to help combat the disease and satisfy clients’ demands. However, if medical attention is needed, the skin care specialist should work with a physician to provide a complete wellness solution that will achieve maximum results for the concerned individual.
A natural and effective option
It is very important that skin care products for rosacea-affected individuals include ingredients, such as green tea, licorice, chamomile and French rose essential oils, and allantoin, capable of addressing microcirculatory and inflammatory problems. Camouflage makeup is another viable topical option to address visible redness. Makeup, preferably mineral, should be hypoallergenic, noncomedogenic, easy to apply, sweatproof and offer SPF protection. But even if makeup is not worn, conscious sun avoidance and a minimum SPF 30 is highly recommended to preserve the skin’s well-being when outdoors for more than 15 minutes under broad sunlight.
Skin care professionals are the next in line to offer affected clients quality of life and the best relief possible from rosacea symptoms. Many professional skin care brands offer safe and effective tools to control the evolution of rosacea and reduce the skin undermining caused by this disorder. Be sure to check with clients’ physicians if they are being medically treated for rosacea. Then, recommend specifically designed whole skin regimens and treatments to target the condition with effective ingredients. It will help guarantee client satisfaction through visible and measurable results for years to come.
Christian Jurist, MD, is a physician who specializes in esthetic medicine and has belonged to several international esthetic medicine professional associations. After leading a medical esthetics curriculum at Florida College of Natural Health as a faculty member in the United States, Jurist joined Pevonia and Medicalia International as medical director of global education. His long-term experience has comprised multiple face and body therapies, plus many years of teaching experience. He also has written professional articles in recognized media publications, and conducted numerous educational seminars, professional trade show conferences, school classes and special events domestically and worldwide.