It is a well-known adage in medicine that if you have more than one treatment for a disease, you do not have the right treatment. Most medical treatments are based on a knowledge of the nature of the disease being treated. When the cause and course of the disease are well known, a specific treatment is then either developed, or research workers try to find the correct one. As an example, a bacterial infection requires a specific antibacterial agent, and diabetes mellitus requires insulin and dietary control.
Cellulite, however, is a very misunderstood disease—in fact, to a large measure, it is not understood at all. Since no one dies from cellulite, there is no political impetus to fund research about it. Somehow, the untold misery and unhappiness of millions of women does not seem to be motive enough for serious research into cellulite.
Before the most probable cause is examined, this article will explore the current concepts and look at some of the treatments offered. Conventional wisdom suggests that cellulite is a disease of the fatty tissue, and is due to lack of exercise and a poor diet. Most so-called beauty magazines advocate exercise and diet as the only effective treatment. Unfortunately, any woman who has tried these modalities realizes they are next to worthless in regard to cellulite.
Both the circulatory and lymphatic systems are critical to a person’s health, but they play only an insignificant role in the genesis of cellulite. Toxins are blamed for everything from erectile dysfunction to brain tumors, so it is not surprising to see it pop up when cellulite is considered, which is sheer nonsense; none of these advocates of cellulite toxins can name a single one or verify the physiological effects of these toxins on cellulite.
Lipodystrophy suggests that there is something wrong with the fatty tissue. The displaced water theory has been around for many years, and goes along with intercellular fluid accumulation. Trauma as cause fits into this category, as does fibrosis.
Current treatments based on these theories all produce some “emperor’s clothes” effects and perhaps some visual improvement, which, at best, is temporary. No amount of pressure, suction, heat, massage, infrared or wrapping will have a lasting effect on the basic cause of cellulite. The newer modalities, such as laser therapy, high frequency energy and microcurrent, can have a positive effect as adjunct treatments, but they are not effective as sole treatment methods.
Basic facts about cellulite
- Only women get true cellulite. It requires a serious systemic disease or gross obesity for men to have even mild cellulite. The true incidence in men is not really known, but, judging from reported cases, it must be insignificant.
- Cellulite has a hereditary component that may be quite complex; to date, it has not been studied. For example, Asian women do not have a significant tendency toward cellulite.
- Cellulite affects only the buttocks, thighs and legs to about four inches above the knees. Pseudo-cellulite may affect other areas in women later in life.Cellulite is a hormonal disease, sparked by estrogen and driven by the enzyme collagenase.
- Cellulite is a treatable disease, but not curable with current biological knowledge.
Cellulite as a disease
A diseasea, as defined by the dictionary, suggests cellulite has several components of a true disease. 1. It is a pathological process (the destruction of collagen); 2. It is part of an organ (the skin); 3. It has various causes; and 4. There are specific signs and symptomsb present. These findings shall be explored in more detail as the pathogenesis of cellulite is examined.
Anatomical basis of cellulite
In the year 2000, I wrote an article about cellulite for Skin Inc. magazine that detailed the basic anatomical structures involved in cellulite.1 In that article, the current literature was reviewed and fundamental facts on the fat in cellulite were detailed; that same data will not be presented in this article.
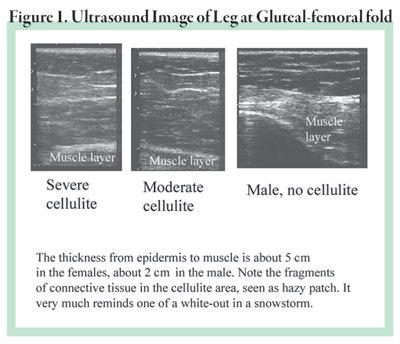
Cellulite is a disease of the connective tissue, otherwise known as collagen. Many articles, both scientific and popular, describe the anatomy of cellulite in an erroneous manner. For example, the upper leg starting from the outside consists of the epidermis, dermis, fatty layers and muscle layer. There are two fatty layers separated by a band of tissue known as fascia. There is little or no difference between women and men in these structures. The fibrous bands that separate the fat into compartments are called trabeculaec. They are somewhat thicker and stronger in a male as seen by ultrasound in Figure 1. Notice the fragmenting of the connective tissue throughout the dermis and subdermis.
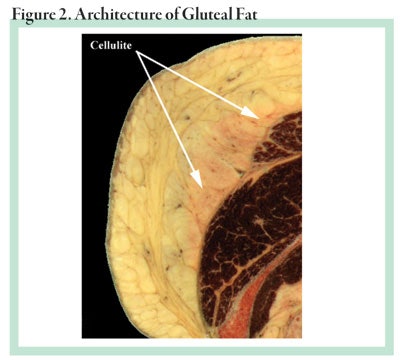
The fatty tissue is composed of exactly the same fatty acids in both sexes and is the same as other fat tissue throughout the body. The major difference is that fatty tissue in the thighs and buttocks contains more alpha-2 receptors than the other anatomical regions. The alpha-2 receptors are inhibitory to lipolysis, the utilization of fat. This fat is reserved for the potential nourishment of a baby during hard times when food is scarce. Only under these conditions, or during extreme starvation, will it be mobilized. Figure 2 shows the architecture of gluteal fat. Please see the January 2000 Skin Inc. magazine article about cellulite for more details about the structure and anatomy of the fatty tissue.1
Hormones, the menstrual cycle and enzymes
Part of the magic of birth is the mystery of conception. Essential to a successful pregnancy is a viable implant of the fertilized egg. To achieve this perfect state, the body will prepare a new endometrium each month for a possible pregnancy. In her child-bearing lifetime, a women may have 400 or more menstrual cycles. It is the enzymes that build up and destroy the endometrium each month that account for the existence of cellulite in women. An understanding of this process requires a familiarity with the biology of the menstrual cycle, so a brief review is in order.
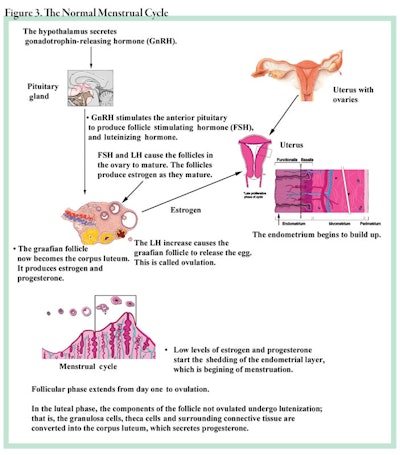
The normal menstrual cycle. The uterus is a muscular structure that is lined with a highly vascular and proliferative tissue called the endometriumd. Each month, under the hormonal influence of follicle-stimulating hormones (FSH), the ovary will begin to ripen and extrude an egg (the ovum). This same hormone will influence the endometrium to start a new cycle of growth. All of this process starts in the hypothalamus, where the specific stimulating hormones originate to direct the pituitary gland to produce the FSH and the luteinizing hormones (LH) needed to prepare the endometrium by directing the ovaries to secrete the female hormones, estrogen and progesterone. Figure 3 illustrates the process in detail. At the end of this phase, the endometrium must be shed if no pregnancy has occurred, and this is the very process that also initiates the condition known as cellulite.
Matrix metalloproteinases (MMPs). When pregnancy does not occur, the sex hormones, estrogen and progesterone fall to very low levels. This initiates a series of events that removes the endometrium by a collagenolytic process called shedding. In this process, specific enzymes, known as matrix metalloproteinases (MMPs) cleave to the collagen fibers and break them down into peptides and amino acids, to be recycled in the metabolic pool. These same enzymes are also responsible for the degradation of other type I collagen structures elsewhere in the body, particularly in the thighs and buttocks—the cellulite area.
This article cannot focus on MMPs in a comprehensive manner, but the basics must be covered in order to allow for a full appreciation of the real nature of cellulite. The four classes of MMPs are the collagenases, gelatinases, stromelysins and membrane-type enzymes (MT-MMPs). All these enzymes share certain characteristics: 1. They all contain zinc metal at the active site; 2. They are synthetized in an inactive form, known as a preproenzyme, and secreted into the extracellular matrix (ECM); 3. They are activated in the ECM; 4. They recognize and cleave the ECM components; and 5. They are inhibited by both serum-borne and extracellular-specific MMP inhibitors. Following are a few of the MMPs and their substrates.
- The collagenases are grouped as MMP-1, MMP-8 and MMP-13. These MMPs can cleave many types of collagen, including types I, II, III, V and XI, which are fibrillare. When these collagen types are cleaved, they become more soluble and form gelatin.
- The gelatinases, MMP-2 and MMP-9, can now take over and attack type IV collagen—the basement membrane of the epidermis—fibronectin and laminin.
- The MMP-3, MMP-7, MMP-10 and MMP-11 attack similar proteins and peptides.
- The metabolic function of these enzymes is quite diverse, because they not only attack connective tissues, but also can direct cell growth by regulating the amount of growth factor bioavailability.
- The MT-MMPs appear to have a key role in this regulation, as well as in controlling other MMPs.
- TIMPs are tissue inhibitors of MMPs. There are four types: TIMP I, TIMP II, TIMP III and TIMP IV.
The menstrual cycle and MMPs
Keep in mind as you read this section that menses occurs each month, and the rise and fall of these enzymes is critical to both ovulation and menstruation. Cellulite is a spin-off process of these enzymes, as are many of the other connective tissue disorders. Ovulation is a major process necessary for an eventual pregnancy. In Figure 3, the process is illustrated and following are the steps.
1. LH initiates a biochemical pathway that stimulates the production of progesterone, cytokines and prostaglandins.
2. These biochemical agents act on granulosa cells and theca cells to produce MMPs and TIMPs.
3. The MMPs destroy the follicle permitting the egg to be released.
4. The TIMPs may orchestrate the formation of the corpus luteum by controlling cellular proliferation and steroidogenesis.
There are many steps and a great deal of information, but for the purpose of this article, this is all you need to remember.
Although quite a bit is known about the physiology of the menstrual cycle, science is very far from understanding everything. For instance, it is not known how estrogen is related to MMP production and utilization.
Following the late secretory phase in the menstrual cycle, there is a fall in the plasma levels of estrogen and progesterone, which is believed to be a critical—if not pivotal—step in the cycle leading to actual menstruation. Keep in mind that the endometrium is a thick mass of collagen and blood vessels, and it needs to be shed within a matter of days to make way for the new growth of endometrium. This requires a vigorous and swift lysis of the interstitial matrix by MMPs under tight control. Although the entire answer is not known, it is known that the fall level of the ovarian steroids, estrogen and progesterone, initiates the stimulation of endometrial fibroblasts to secrete MMP-1. This secretion appears to be controlled by an interleukin, specifically interleukin IL-1alphaf. This occurs around the perimenstrual phase, probably five to seven daysg.
This is the key step relating menses to the genesis of cellulite. MMP-1 is triggered to form in and be secreted from the fibroblasts not only in the uterus, but also in other fibroblasts of the body. This statement is based on the fact that women get MMP-associated diseases, such as temporomandibular joint disease2 and anterior cruciate ligament disease.3 In the case of the adipose tissue in the thighs and legs, the main target is the connective tissue, that is, the fibrous bands that support and separate the fatty tissue into discrete compartments. As these bands are broken down in a manner not yet known though it appears rather random, the fatty tissue will move upward and laterally to fill the space available. The bands that are not destroyed remain attached to the dermis and create an undulating pattern of hills (no bands) and valleys (bands still attached).
Let’s step back and look at this devastation. Here is a picture of what the inside of a cellulite area may present to a viewer.
The trabeculations, or fatty septae are fragmented in a chaotic fashion; fatty tissue is no longer confined to anatomical compartments; fat is allowed to expand in a nonphysiological manner, even producing new fat cells in the newly created spaces; every month, a new MMP insult assails this damaged tissue making it quite impossible to repair; a shattered landscape results with great globs of unorganized fatty tissue and fragmented collagen littering the interstitial spaces.
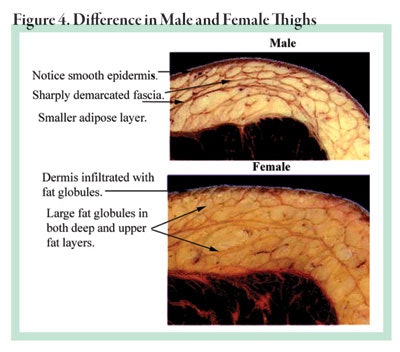
Figure 4 shows the difference between a male thigh without cellulite and a female thigh with cellulite. The fine details of cellulite are not visible in these sections as they are “fixed” tissue; that is, they are essentially frozen in time by chemical means called fixation. Notice that the thickness of the female thigh is much greater than the male thigh, and that the fat globules are larger. In addition, the collagen bundles are more defined in the male than in the female.
In part two of this article, learn about the pathological changes in cellulite tissues, as well as a new treatment for cellulite.
REFERENCES
1. PT Pugliese, Cellulite, Skin Inc. magazine, 60–66 (Jan 2000)
2. G Guan et al, Estrogenic effect on swelling and monocytic receptor expression in an arthritic temporomandibular joint model, J Steroid Biochem and Molecular Bio, (97) 241–250 (2005)
3. RJ Clark et al, The menstrual cycle, sex hormones, and anterior cruciate ligament injury, J Athl Train, (37) 275–278 (2002)