The term “sensitive skin” has become very common—approximately 57% of people say that they have skin sensitivity, yet few are actually born with it.1 Only 2% of adults in America actually have sensitive skin.1 Sensitive skin is characterized by excessive dryness, stinging, burning, redness and tightness, and is often a reaction to certain skin care products or other products that come in contact with the skin. It has a tendency to blush and flush easily because it has more reactive blood vessels than normal skin. This type of skin may also react with pustules, skin bumps and skin erosion.
Sensitive skin can be genetic and inherent, according to race, age and gender, but the majority of people affected by sensitive skin have become so due to environmental or lifestyle factors. The skin’s main function is to protect; however, exposure to the factors that cause sensitivity can compromise its ability to function optimally. The first step toward conquering skin sensitivity is education.
If your skin is sensitive, chances are that it has a thinner strateum corneum, a weaker natural defense barrier of lipids and may have more dermal appendages, such as hair follicles, and sebaceous and sweat glands. These characteristics of the skin’s structure result in heightened permeability and less protection against irritating ingredients or pollutants, as well as an increase in moisture loss.
Triggers
As mentioned, external factors, such as environmental aggressors and exposure to irritating ingredients and chemicals, are known to bring on skin sensitivity. With these factors, the skin may often return to its normal state after exposure to the irritants has ceased. Throughout time, however, these factors compromise the integrity of the epidermis. Harsh cleansing, overexfoliating and exposure to pollutants and irritants can allow for minute cracks—invisible to the naked eye, but large enough to allow the penetration of the epidermis—causing inflammation. Skin can become more sensitive as natural secretions diminish and the subcutaneous fat layer thins. Harsh ingredients should be avoided in order to keep the barrier intact, including strong acids and alkalis, chemical sunscreens, surfactants, penetration enhancers, benzoyl peroxide and hydrogen peroxide. Hormonal changes that come with puberty, pregnancy and menopause may also trigger sensitivity.
Caring for sensitive skin
The goal in caring for sensitive skin is to smooth, calm and hydrate. Sensitive skin can be treated using calming ingredients, such as seaweed, olive oil, olive leaf extracts, green and white tea and allantoin. Natural antioxidants help to prevent the free-radical damage that triggers sensitivity. Boosting the skin’s own protective lipids by adding essential fatty acids, gamma linoleic acid and hyaluronic acid can provide the raw materials needed by epidermal cells to generate lipids.
Those with sensitive skin must pay special attention to their skin care regimens. Fragranced products can irritate the skin further, and facial cleansers that contain detergents and soap have high alkaline levels, and are drying and irritating to the skin.
Moisturization is key when it comes to sensitive skin. Products that create a proper lipid barrier and have moisture-boosting ingredients are the best. Also, advise clients to wear a foundation or base containing an SPF to avoid damage from the sun. For more tips, see Cosmetic Tips for Sensitive Skin.
Rosacea
Rosacea, a condition associated with sensitive skin, is common—and commonly misunderstood—although it affects more than 14 million Americans today, according to the National Rosacea Society. What is rosacea, and why is it often misdiagnosed or even undiagnosed?
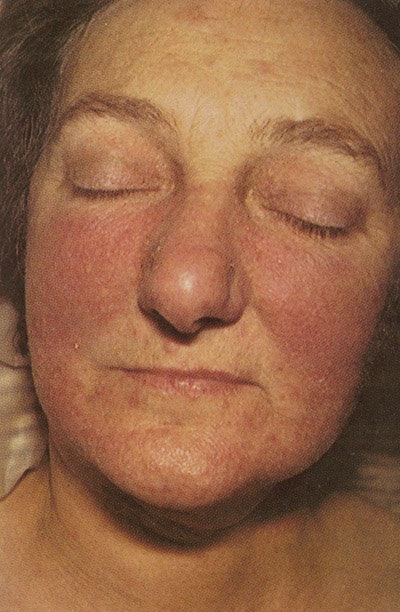
It is a chronic neurovascular disorder that causes red, thickened, inflamed skin. Characteristics include telangestasia, or broken blood vessels, and pustules, which is why the condition is often mistaken for acne. Rosacea usually occurs on the face, but may also affect the neck and upper chest. A physician will diagnose rosacea by checking the skin, eyes and chest for symptoms. It is helpful to know when the symptoms first occurred and how often they take place.
Rosacea manifests in stages. Early signs normally begin by the age of 20–30, with recurring episodes of blushing that eventually become persistent dark red erythema, mainly in the nose and cheeks. The condition may evolve into papules (small red bumps), pustules, burning and soreness in the eyes and eyelids, burning and stinging sensations on the skin and, in some more extreme cases, red, knobby bumps on the nose and cheeks.
It is not entirely known what causes rosacea, but it is carried on genetically and is most common in fair-skinned individuals, occurring more often in women than men. Rosacea flareups are usually triggered by external factors that cause blood vessels to dilate, such as alcohol use, sun exposure, stress and spicy foods. The leading factors of rosacea include the following.
- Vascular endothelial growth factor (VEGE). VEGE is the creation of blood vessels caused by heat and sun exposure, and it may cause spider veins.
- Demodex. People who suffer from rosacea are more susceptible to mites known as Demodex. The bacterial flora that live on mites causes rosacea by secreting the enzyme that helps to eat food from the skin.
- Lipase. Lipase is an irritating enzyme that helps breakdown lipids. The Demodex mites secrete this enzyme resulting in irritation and redness.
Although there is no cure for rosacea, there is treatment. As an esthetician, it is a good idea to work with a dermatologist when treating more severe cases of rosacea. A physician can prescribe medications, including antibiotic creams and pills, to address redness, pimples and eye problems. Red bumps on the nose normally do not respond well to antibiotics. Isotretinoin and tretinoin can be prescribed, as well as other topical medications that are used to treat acne. Surgery, such as dermabrasion, cryosurgery and laser surgery, can help treat the cosmetic effects of advanced rosacea.
Additionally, there are steps to take to help prevent initial rosacea flareups. Identifying your clients’ triggers is extremely important, and avoiding the catalysts will help prevent the results. See Common Rosacea Triggers.
In addition to consulting with a physician, estheticians can practice the following precautions when working with clients who suffer from rosacea:
- Avoid heat, steam and sunlight.
- Avoid vasodilators and irritants.
- Avoid stimulating massage movements.
- Avoid flushing and blushing agents, such as AHAs and retinol.
- Introduce nonsteroidal anti-inflammatories, such as chamomile and tea blends.
- Limit ingredients and use the same line.
- Choose multifunctional products.
- Recommend sunscreen with a physical barrier, such as titanium and zinc.
- Use cooling treatments, such as freeze-dried facials, cold compresses and cool mists.
In addition to these techniques, it is important to provide gentle, cooling treatments. Try using an atomizer with a few drops of an antioxidant-rich toner for a cooling mist that’s very hydrating and soothing for clients. Implement lymphatic massage to reduce swelling and inflammation in order to detoxify and purify the skin. Apply light effleurage movements, and avoid unnecessary massage and rubbing of the face.
Remember, when it comes to skin care, the most important steps are to provide consultation, diagnosis and recommendation of treatment and at-home care.
REFERENCE
1. N Singer, Face it Princess, Your Skin is Probably Quite Common. New York Times, Oct 13, 2005
GENERAL REFERENCES
C Sweeney, In a Perfect World, Rosacea Remains a Problem. New York Times, April 24, 2008
G Plewig and A Klingman, Acne and Rosacea, 2nd completely revised and enlarged edition. Springer-Verlag, New York,1993