Based on current estimates, 8,420 people are expected to die from melanoma this year. In an effort to reverse this sobering trend, dermatologists and the scientific community alike are continually developing new diagnostics, refining detection guidelines and providing patients with the tools they need to properly examine their own skin for signs of skin cancer.
Speaking on Nov. 13, 2008, at the American Academy of Dermatology’s Skin academy, dermatologist Ellen S. Marmur, MD, FAAD, chief of the division of dermatologic and cosmetic surgery at The Mount Sinai Medical Center in New York, presented the latest advances in diagnosing skin cancer and the Academy’s new detection strategies that emphasize the importance of patient involvement.
“There are some exciting innovations in diagnosing skin cancer that can help us detect skin cancer early, when it is most treatable,” said Marmur. “Even simple detection tools designed by the Academy that patients can use in their own homes can save thousands of lives.”
New technologies for diagnosing skin cancer
Dermatologists traditionally diagnose skin cancer by evaluating the skin using a clinical examination and, if necessary, a magnifying device and then biopsying any suspicious lesions. Now, technological advances in computers, lasers and other polarizing light sources are providing dermatologists with tools to enhance the evaluation of suspicious lesions and, in some cases, decreasing the number of biopsies needed for an accurate diagnosis. The idea is to hone in on suspicious lesions earlier and with more specificity.
One of the newest technological developments in the fight against skin cancer is the use of sophisticated imaging to scan and enhance certain features of suspected lesions. Similar to how a computerized tomography (CT) scan highlights areas of the brain for abnormalities, imaging devices can now work on the skin to help detect cancerous tissue.
Another exciting technology dermatologists are using to evaluate suspected skin cancers is a hand-held light device known as dermascopy that can look at the pigment of the skin through specialized filters that magnify and polarize lesions. For example, similar to how filters are used on cameras to create certain backgrounds, filters are used on this device to enhance certain features of lesions - such as brown or red background colors that could indicate a melanoma (the deadliest form of skin cancer).
Marmur noted that one of the main benefits of dermascopy is the ability to immediately evaluate a potential melanoma based on its magnified characteristics, which could help decrease the number of biopsies needed to make an accurate diagnosis, or can push the physician to biopsy a borderline lesion that appears more suspicious with the assistance of the dermatoscope.
In addition, newer computer systems are being used in conjunction with hand-held photography devices to more accurately diagnose melanomas. For example, the photo device takes a digital picture of the suspicious lesion, which is then magnified on the computer screen for closer examination. The computer system also contains a database of characteristics of approximately 100,000 evolving melanomas, which the lesions are then graded against to see if certain features score high enough on the scale to warrant having a biopsy.
“With the improvement of early detection methods, we are finding an increasing number of smaller skin cancers,” said Marmur. “We know from experience that detecting skin cancer in its earliest stage means better cure rates and survival rates. Prognosis plummets as the depth of melanoma increases even by the smallest increment of one millimeter.”
New self-exam tools
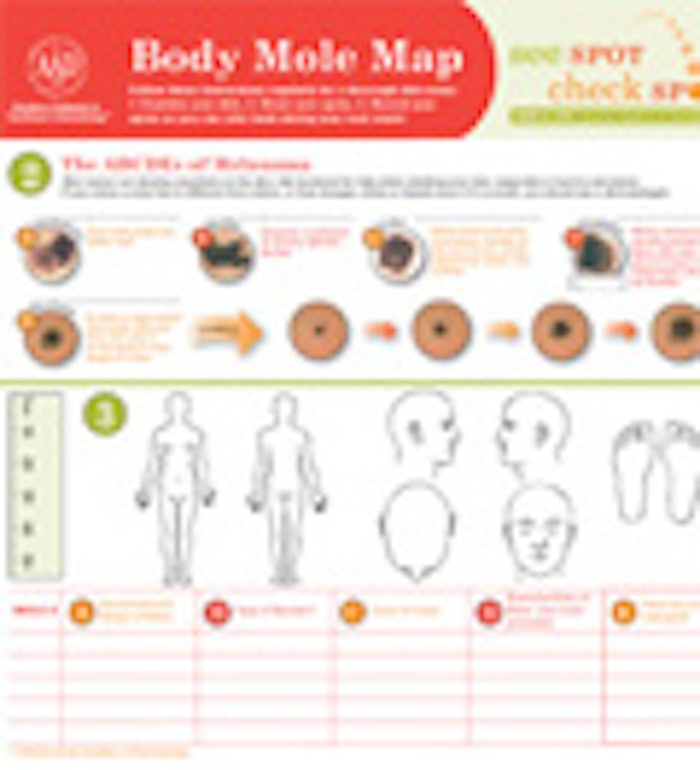
Since skin cancer is the only cancer you can see on the surface of your skin at its earliest stage, performing regular skin self-examinations is an easy way to detect any suspicious spots that could be cancerous. To enhance a patient’s ability to detect the warning signs of skin cancer, the Academy is refining the ABCDs of melanoma detection by adding an “E.” The letter “E” stands for Evolving - a mole or skin lesion that looks different from the rest or is changing in size, shape or color. This is in addition to other qualities of moles for which individuals should check their skin - Asymmetry (one half unlike the other half), Border (irregular, scalloped or poorly defined), Color (varies from one area to another; shades of tan and brown, black; sometimes white, red or blue), and Diameter (the size of a pencil eraser or larger). If a mole exhibits any of these characteristics, it should be brought to a dermatologist’s attention.
An analysis of 2001-2005 data from the Academy’s National Melanoma/Skin Cancer Screening Program supports the need for people to watch their moles for changes. A study of the data published in the July 2007 issue of the Journal of the American Academy of Dermatology found those who indicated they had a mole that changed recently in size, color or shape were two times more likely to be diagnosed with a suspected melanoma.
“Some melanomas don’t show any other abnormalities except that they are evolving over time,” said Marmur. “It’s not unusual for people to wait until a melanoma has grown significantly to see a dermatologist, and unfortunately, that sometimes means the cancer has spread to other areas of the body. I am confident lives will be saved by encouraging people to bring their evolving moles to the attention of a dermatologist. And I have been able to save lives purely because a partner or spouse has detected a changing lesion on someone who rushed in for a biopsy and curative surgery.”
Marmur explained she sees numerous patients who say that they have had a mole forever, but that it recently started bleeding and then ultimately turns out to be a skin cancer. She added that a classic example of an evolving skin cancer is a man who notices a mole that begins bleeding while he is shaving. This can be a basal cell carcinoma, a squamous cell carcinoma or a melanoma. All three are serious and can be cured if caught early.
“Melanoma can be on the skin for a long time before it ‘misbehaves’ and gives patients a clue that it may be a lesion that needs to be addressed,” said Marmur. “We find that people who check their skin regularly - looking for the warning signs of skin cancer and taking note of any changes - are more likely to spot skin cancer in its earliest stages before it spreads.”
The Academy’s Body Mole Map is a tool individuals can use to track their moles. The map provides information on how to perform a skin exam, images of the ABCDEs of melanoma and space for people to track their moles to determine any changes over time. Free downloads of the Body Mole Map are available at www.melanomamonday.org.
Marmur also encourages her patients to involve a family member or partner in skin exams, which can help people thoroughly examine their skin in hard-to-reach spots and help them decide if a lesion seems to be evolving over time. In her practice, Marmur estimates that patients report that they are getting a suspicious mole checked at the urging of another person about five times per week - with men representing the largest group of referrals.
Involving a partner in the self-examination process can improve the early detection of skin cancer. As such, the Academy is encouraging people to “Screen the One You Love.” While candy and flowers are short-term gifts, the gift of a skin examination is a gift of life and health. Popular holidays, such as Valentine’s Day (February 14), Mother’s Day (May 10), Father’s Day (June 21) and Grandparents Day (September 13) are reminders for people to check their loved ones’ skin for suspicious moles using the Academy’s Body Mole Map.
“People sometimes get confused by what to look for on their skin, and that could result in them ignoring any potential red flags that might be starting to crop up,” said Marmur. “So I always tell people to get to know their skin and if something is bleeding or doesn’t look right, then see a dermatologist. Whether or not you have a partner available to assist you with your skin self-exam, you should make skin self-exams part of your regular health regimen."
For more information about skin cancer, please visit the SkinCancerNet section of www.skincarephysicians.com, a Web site developed by dermatologists that provides patients with up-to-date information on the treatment and management of disorders of the skin, hair and nails.










