
Close to 85% of people will experience some form of acne in their lifetime.1 According to the American Academy of Dermatology, acne is the most common skin disorder in the United States, affecting 40 to 50 million people at some point in the lives.2 Whether in a spa, salon or medical spa setting, treating acne can be one of the most rewarding experiences for an esthetician.
While there are many medical and at-home interventions for acne, the treatment room is the ideal setting for acne treatment for many reasons, including the following:
Licensed professional. In a spa, a licensed skin care professional can provide immediate help for the acne breakout.
Stress reduction. A spa provides a haven for relaxation to reduce stress, a key trigger for acne flare-ups.
Education. A treatment room is the perfect forum for educating the client on the benefits of proper skin care, a healthy diet and lifestyle choices that can help reduce acne flare-ups in the future.
There are many myths and misconceptions about acne, particularly when it comes to age and diet. Improper at-home treatment can even lead to permanent damage of the skin. Here, we’ll review the facts about acne, explain the proper professional treatment, and provide the essential information needed to demystify the many myths surrounding the skin condition.
The Cause of Acne
When people think of acne, they think of teenagers, but acne can affect many people through adulthood as well. Some estimate as many as half of all adult women experience some form of acne due to an increase in androgen and a decrease of estrogen in peri-menopause.
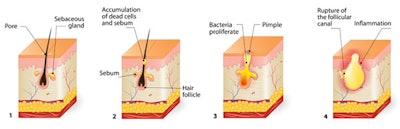
Acne is an inflammatory lesion of the sebaceous glands. The first signs are usually during puberty with the increase in androgen hormones. Fluctuations in this hormone can stimulate the amount of oil produced by the sebaceous glands, which create sebum at the root of the hair follicle in the dermis. Throughout life, hormonal fluctuations, pharmaceutical agents, stress, heat, humidity and dietary agents can contribute to sebaceous gland stimulation and bacterial growth.
Three factors present on the skin can cause acne: sebum, bacteria and enclosure. When these factors are encountered together, it creates an environment for inflamed, irritated and congested skin.
Sebum. This oily substance lubricates the surface of the skin to help prevent surface dehydration. When there is an over-abundance of sebum, it fills the sebaceous duct. This serves as a nutrient for bacteria, which creates an environment for clogged pores.
Bacteria. Growth of Propionibacterium acnes (P. acnes) can cause acne vulgaris, the most common form of acne.
Enclosure. When the wall of the sebaceous duct and the formation of a keratinaceous plug prevents wicking of sebum, a closed environment results.
It’s important to remember these skin formulas when encountering these factors on the skin:
Bacteria + Sebum = Irritation
Enclosure + Sebum = Closed Comedone
Enclosure + Bacteria + Sebum = Full-blown Acne
Oil mixes with perspiration, helping to retain water in the tissue As the ducts of these glands become plugged with the waxy oil, comedones (black heads) and milia (white heads) form. These can become infected by bacteria, causing welts, deeper lumps and pimples (cysts or nodules).
Types of Acne and Lesions
There are many types of acne, which are characterized by their causes. Some of the most common forms include: genetic acne (Acne conglobata); acne from abrasive cleansers (Acne detergents); acne from the psychosomatic picking of the face (Acne excoriee); acne from excessive sun exposure (Acne mallora); acne from mechanical irritation (Acne mechanica); acne from exposure to industrial chemicals (Chloracne acne); severe acne from sebum, dead cells and bacteria (Cystic acne); acne from comedogenic cosmetics (Acne cosmetica) and acne from androgenic male hormones (Acne vulgaris).
Non-inflammatory Acne
The first stage of an impacted follicle can be referred to as a micro-comedone. This comedo formed below the epidermis cannot be seen by the naked eye. It feels like a small hard bump. As it enlarges, it looks like a tiny white bump just below the surface of the skin.
As the bacteria digests sebum, fatty acid waste is produced that irritates the lining of the follicle, causing a proliferation of cells to accumulate in the impacted follicle. Non-inflammatory lesions result with closed comedones or white heads, a firm white papule.
Inflamed lesions turn into open comedones, where sebum and dead skin cells comprise this hard plug. This is the mildest form of acne.
Inflammatory Acne
When inflamed lesions eventually turn into open comedones and expel their contents, inflamed lesions may also result, whereby the follicle wall ruptures forming a papule. These inflamed lesions, or small, solid slightly raised areas of the skin, are less than half-an-inch in diameter. They can be varied in appearance, rounded, smooth or rough, skin-colored or pink, red or brown.
Milia, or epidermal cysts, are small, firm white papules usually found in clusters on the upper cheek and around the eyes.
White blood cells invade the area and inflammation ensues. If the break is close to the surface of the skin, a pustule results. This small, pus-containing skin blister is often found at the opening of hair follicles. It has more visible inflammation than a papule.
When white blood cells invade a papule, if the break is deeper, a nodule forms. These large, painful solid lesions extend deep into the skin.
In some cases, a membrane entraps the infection and a cyst forms. Cysts are inflamed pus-filled lesions.
Acne Treatment Protocol
Before starting, make sure the treatment room and all instruments are clean and sterilized. This should be done in all treatments, but it is especially important for treatment of acne, where lancets and comedone extractors (where allowed by state law) can make the skin more susceptible to infection.
Excess sebum must be addressed in all acne patients. Excess sebum is the catalyst for the series of events that result in acne and is associated with enlarged pores, follicle congestion and an oily T-zone. Therefore, the first step must be to address excess sebum production and help maintain proper moisture levels.
Cleanse. Cleanse skin using a soap-free formula that deep cleanses without causing dryness, preferably one that contains salicylic acid, which neutralizes bacteria while gently exfoliating the skin. Cleansers should also contain soothing and antioxidant ingredients, such as seaweed and green, white and rooibos teas.
Desincrustation. You can gently steam the face, then follow with a desincrustation mask.
Desincrustation is a process of softening the keratinaceous horny plug to allow extractions to proceed easily with minimal trauma to the surrounding tissue. This can be achieved by using the proper desincrustation mask or gel.

The efficacy can be increased when used in conjunction with galvanic current. Desincrustation masks should both soften and purify the skin. Seaweed-based ingredients are particularly effective for this because of their affinity to skin composition. This can be combined with salicylic acid, as well as soothing and purifying ingredients, such as sage, aloe and rosemary. The mask can be left on for 8 to 10 minutes.
Extractions. For extractions, cleanse and sanitize hands thoroughly and use vinyl gloves. Blackheads can be manually removed using fingertips, exerting pressure on the skin surrounding the blackhead or comedone, then lifting the blackhead from the follicle opening gently. Comedone extractors can also be used for this or a sterile cotton swab. It is important to use the sides of the fingertips to exert pressure on the skin surrounding the comedone, not the fingernails, as this can dig the impaction deeper into the skin.

For removal of milia or pustules, estheticians can use lancets. Check with your local state board to see if it is permissible. Cysts and nodules must be treated by a dermatologist. As a licensed esthetician, you can still administer acne treatments that will help with cystic skin, but you won’t be able to remove these lesions.
Remember to hold the lancet parallel to the skin and gently pierce the skin in a horizontal motion at the follicle opening. Pricking into the skin in a downward motion can cause scarring. After piercing the skin horizontally, wrap the index fingers with cotton or use sterile cotton swabs, gently pressing down on both sides of the milia. Lancets can never be reused and must be thrown away in a sharp box.
Extractions should never take more than 10 minutes during a single treatment. If the contents of the comedones do not easily expel, leave it for the next treatment. Comedones did not occur in one day, and many times it will take more than one treatment to clear them up.
Calm skin. Follow up with an astringent that helps restore the pH balance. A client should never leave the salon with red, irritated skin after an acne treatment. You should always follow extraction with antibacterial, anti-inflammatory mud mask made from ichthammol to restore moisture and reduce redness. A calming calamine mask can restore skin balance.
It is key that the client’s skin is moisturized upon completion of the facial treatment to further reduce dryness and irritation. Oily skin can still be dehydrated skin. Use a mattifying moisturizer that will restore lipids yet reduce oil and shine.

Integrate technology. A electric therapy machine can be used to augment the salon or spa procedure. These high-frequency UVC germicidal rays can be applied to the skin to reduce bacteria, decrease inflammation, allow for faster healing time of lesions and prevent secondary infections. Contraindications of using this type of device would include pregnancy, high blood pressure, heart conditions, epilepsy, asthma and dental patients with a high content of metals in their mouth.
Lifestyle Education
Education and knowledge are key in treating acne. The client should be advised of the importance of professional skin treatments and following a home care program designed for their acne issues. Discuss the following points for better home care.
Don’t pick. Break bad habits, such as picking and squeezing the skin. Picking can spread acne-causing bacteria, and squeezing can spread infected material deeper into the skin, causing more inflammation and even scarring. Acne will go away, but scars will not.
Don’t over-cleanse. Over-cleansing can be detrimental to acne-prone skin as well. This can further irritate the skin, stripping essential moisture, causing inflammation and additional risk of infection.
Don’t neglect your diet. New research has found that dairy and fermented or yeast-based foods can exacerbate acne conditions. These include aged cheeses, highly processed milk, wine, beer, champagne and mushrooms. Skin care experts now recommend probiotics to counteract unhealthy bacteria living in the stomach lining and the resulting inflammation that can increase acne flare ups as well. Ingesting spirulina to rid the body of toxins and bolster free radical protection is now an established protocol as well.
Don’t tan. Avoid sunbathing, and not just because of the damaging UV light. Once considered part of an acne treatment program, UV light can initially dry up excess sebum and reduce pustules, but can lead to a cascade of reactions that actually increase oil production and sebum build-up on the skin.
Better Health and Appearance
Acne treatment is one of the leading reasons clients seek out professional help, and is one of the most important factors in an esthetician’s practice. Performing consistent effective treatments will not only benefit a client’s overall physical health, but bolster their self-esteem. Both of these results are perhaps the most important achievements to which an esthetician can aspire.
References
- K Bhate and HC Williams, Epidemiology of acne vulgaris, Br J Dermatol, 168(3) 474-85 (2013)
- DR Bickers et al, The burden of skin diseases: 2004 a joint project of the American Academy of Dermatology Association and the Society for Investigative Dermatology, J Am Acad Dermatol 55(3) 490-500 (2006)











