The skin disorder keratosis pilaris (KP)—sometimes called follicular keratitis—is so common that it may be seen almost daily in a busy esthetic practice. Although never fatal, not contagious and medically harmless, it can be emotionally distressing because of its appearance. This is especially true in adolescents, where it is most common. Clients with KP may call it “bumpy skin” because of its appearance. Even though they may not like its appearance, they may have been told by their doctor that nothing can be done for it. However, there are a number of esthetic treatments that can help eliminate and prevent KP.
Causation and Occurrence
KP truly is common, as it affects nearly 50% of the population.1 In addition, it is genetic, and those that get it inherit abnormal keratinization of the skin’s hair follicles. It is an autosomal dominant with incomplete penetrance.2 This means that if one parent has the gene, there is a 50% chance that each of their children will have the gene. However, not every person with the gene will exhibit the physical characteristics of the disorder.
Symptoms appear in adolescence or before 2 years of age and may gradually decrease until they become less noticeable by the age of 30. But many adults still have symptoms well into old age.
Keratinization within the hair follicles causes accumulation of stratum corneum keratin within pores and leads to the typical appearance of bumps on the skin.3 These bumps have been likened to “goose flesh” or “plucked chicken skin.” Hairs often become stuck below the keratin plug, causing enlargement of the bump. The exact reason for the buildup of keratin is not known. There is an association with allergic diseases such as atopic dermatitis but also with asthma and allergies.4 There may also occasionally be an inflammatory component with associated redness at the pilosebaceous unit. Sometimes, the small bumps are mistaken for acne, but the comedone of acne is absent in KP. There is no ethnic predominance, and KP is found over the entire world, though it may be slightly more common in women.2

Symptoms
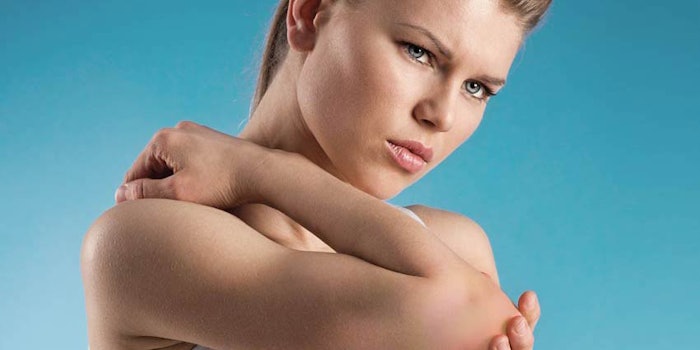
Usually, there is no discomfort associated with keratosis pilaris. Itching may be present, especially if there is associated inflammation. The most common complaint centers around the skin’s appearance and a desire to lessen the appearance of the tiny bumps. These are located on the upper arms, thighs, buttocks and/or face. Occasionally, the bumps are reddish or brown in color and are more noticeable. The skin may feel dry or rough over the affected areas.5 Symptoms may be worse during puberty when hormone levels increase. It may be worse in obesity. During times of low humidity, such as in winter, symptoms tend to increase.3
Esthetic Consultation
Clients should first be reassured that this is not a serious disorder. It is never life threatening or medically serious, and it cannot be passed to others. If the individual finds its appearance distressing and wishes improvement, esthetic treatments and topical products are sufficient.
It may be present throughout life, but often the symptoms disappear over the age of 30. It should also be explained that the disorder is common. It is not rare or unusual. Invasive tests are not required, and a diagnosis is made by the appearance of the skin only.
Treatments
Treatment of KP involves two main steps: exfoliation and moisturization. This addresses the keratin plugging of the pilosebaceous unit as well as the associated dry skin. Ongoing esthetic treatments are usually needed because the disorder persists, and symptoms often recur.
Moisturization. Moisturization is definitely helpful, and dermatologists often advise patients to apply generous amounts of humectants several times per day. These should be lipid-rich and non-drying.2 Urea and lactic acid are two moisturizing ingredients recommended by dermatologists.3 Moisturizer should be applied just out of the shower or bath while the skin is still slightly damp.

Exfoliation. Exfoliation helps resurface the skin, removing dead skin and keratin from the pores. Exfoliants recommended include alpha hydroxy acids (AHAs) to increase normal processes of exfoliation and beta hydroxy acids (BHAs) to help clean debris from pores. Care must be taken to avoid aggressive exfoliation; however, because this could increase the inflammatory component. Recommended exfoliants include glycolic acid, mixed fruit acids, salicylic acid or willow bark acid.
Retinoids and steroids. A retinoid such as retinol, adapalene, tretinoin or tazarotene is recommended for the treatment of KP. Topical steroids may also be helpful.4
Lasers. Since the disorder is a cosmetic one, patients rarely desire aggressive treatment. However, fractional laser treatments have been helpful, especially if KP is associated with hyperpigmentation or is more severe.6 Care must be taken when using laser treatments in darker skin types because of the risk of post-inflammatory hyperpigmentation.
Lifestyle
Clients must be advised to continue both exfoliation and moisturization at home to keep KP at bay. Showers should be relatively brief with tepid water. A humidifier may help with dry skin prevention.
Be Diligent
The prognosis in keratosis pilaris is good with or without treatment. Patients usually seek treatment if they dislike the appearance of the bumps on their skin or if they have more inflammation or itching. Many times, symptoms decrease after the age of 30 although it is also common to have some symptoms throughout life. Esthetic treatments and topicals are very helpful and provide the only treatment necessary. However, because symptoms tend to recur, treatments often must continue for years.
REFERENCES
- B Mevorah, A Marazzi and E Frenk, The prevalence of accentuated palmoplantar markings and keratosis pilaris in atopic dermatitis, autosomal dominant ichthyosis and control dermatological patients, Br J Dermatol 112(6) 679-685 (1985)
- https://emedicine.medscape.com/article/1070651-overview
- www.mayoclinic.org/diseases-conditions/keratosis-pilaris/symptoms-causes/syc-20351149
- S Hwang and RA Schwartz, Keratosis pilaris: A common follicular hyperkeratosis, Cutis Sep 82(3) 177-180 (2008)
- www.aad.org/public/diseases/bumps-and-growths/keratosis-pilaris
- www.hindawi.com/journals/bmri/2016/1928540/












