Eczema and psoriasis are some of the most challenging skin conditions encountered by skin care professionals. Often, there will simply be a little red rash on the skin and you may be left scratching your own head trying to figure out how it came to be. Up to 20% of the world’s children suffer from eczema1, 2 and up to 3% of adults suffer from either eczema or psoriasis.3 Given that the world population just reached the 7 billion mark, that’s a lot of people. Eczema, along with asthma and allergies, are on the rise; in fact, eczema is much more common today than it was 30 years ago, especially in children. This rapid spike in apparent incidence is cause for concern, and may be due to many factors, such as inadequate diet, pollution and other environmental stressors. The truth is, it isn’t known exactly what causes eczema or psoriasis. The good news is, more and more is being learned about these inflammatory skin diseases and strategies are being developed to effectively manage their symptoms.
It is significant to note that neither condition is contagious, nor are they infections; and they aren’t transmitted by external contact or exposure. The origins of eczema and psoriasis are genetic; however, the triggers that cause their distressing and visible symptoms may include stress and environmental factors.
Eczema
A rash by any other name is still a rash. The terms “eczema” or “dermatitis” are very broad and can mean a whole family of skin conditions, ranging from dandruff, to contact dermatitis to atopic dermatitis. This can lead to many a confused client and skin care professional. In dermatology and skin care, the word “eczema” typically refers to atopic dermatitis (AD), a chronic inflammatory skin disease. It causes dry, itchy, irritated skin that requires daily care. Genetic defects in eczema result in abnormal skin cell differentiation. During differentiation, keratinocytes move from the basal cell layer of the epidermis through the granular layer to a group of flattened dead cells in the stratum corneum. This process of epidermal differentiation, or keratinization, involves a variety of proteins responsible for different functions at each stage.
One of these proteins, filaggrin, plays a major role in epidermal homeostasis; it has two main functions. First, it stacks the keratin filaments into dense bundles, allowing for easy desquamation. Imagine how much easier it is to move flattened boxes than propped-open boxes. It is then converted into the skin’s natural moisturizing factor (NMF) along with other byproducts. So if filaggrin does not work very well, it can have adverse effects, not only on the process of epidermal differentiation, but also on the skin’s natural moisture levels and protective lipid barrier. This seems to be the biological basis of dry skin.
In the past five years, researchers have established the link between filaggrin mutations and developing ichthyosis vulgaris4, atopic eczema5 and, most recently, peanut allergies.6 Ichthyosis is another skin disease characterized by very dry skin. The word itself is Greek for “fish,” suggesting the scaly nature of the lesions. Indeed, scientists are getting closer to understanding the genetic connection between allergic diseases, bringing hope for a future therapy not only for eczema clients, but also for those with allergies and ichthyosis.
There’s another type of eczema that shows up as the same itchy rash, but does not involve allergic responses. This is known as nonatopic eczema, and it affects millions of adults. Although most—
about 90%—develop atopic dermatitis before age 5, nonatopic dermatitis develops in adolescence or adulthood, typically by age 15.7, 8 These people don’t have heightened allergic responses or specific allergies, but still get dry, itchy skin. Keep in mind that even if a client is classified as atopic or nonatopic, the end result is the same itchy patch of skin, which must be cared for in the same manner.
Psoriasis
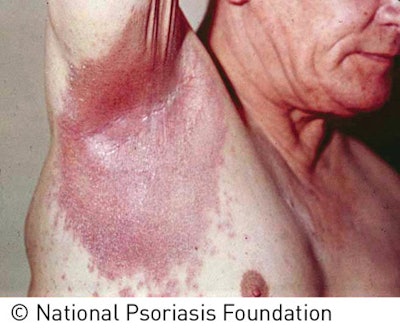
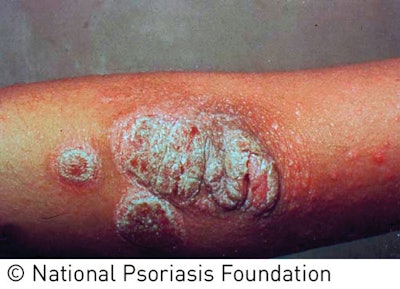
Psoriasis has been confused with eczema, lupus, boils, vitiligo and leprosy. Because of the confusing connection with leprosy in ancient times, psoriasis sufferers were even made to wear special suits and carry a rattle or bell, like lepers, announcing their presence. Only in the 19th century was a distinction made between psoriasis and leprosy, alleviating some of the psychosocial impact of this highly visible and distressing skin disease.9 As with eczema, it presents as itchy, red skin and involves altered immunity. However, its complexities reach far beyond the surface of the skin. People with psoriasis have an increased risk of cardiovascular disease, metabolic syndrome, obesity and other immune-related inflammatory diseases—even cancer. The mysteries behind this complicated and debilitating skin disease are only beginning to be unraveled. Psoriasis is a chronic, inflammatory multisystem disease affecting 1–3% of the world’s population.3 Whereas the rashes on eczematous skin can have irregular edges and texture, psoriatic lesions tend to be more uniform and distinct. Red or pink areas of thickened, raised and dry skin typically present on the elbows, knees and scalp. This presentation tends to be more common in areas of trauma, abrasions or repeated rubbing and use, although any area may be affected. Unlike eczema, psoriasis comes in five different forms: plaque, guttate, pustular, inverse and erythrodermic.
Plaque psoriasis affects about 80% of those who suffer from psoriasis, making it the most common type. You’re likely to encounter this type in a skin care facility, so it’s important to know how to identify and understand it to help you better manage your client’s needs. It may initially appear as small red bumps that can then enlarge and form scales. The hallmarks of this type are raised, thickened patches of red skin covered in silvery scales. The other types are less common and present inflamed skin with red bumps; pustules; cracked, dry skin; and even burned-looking skin. Clients will most likely be under a physician’s care, who will diagnose the type of psoriasis present.
As of today, psoriasis has no cure. A single cause of the disease has yet to be uncovered, but it is known that developing the disease involves the immune system, genetics and environmental factors. In psoriasis, aberrant immune activity causes inflammatory signals to go haywire in the epidermis, causing a buildup of cells on the surface of the skin. While normal skin takes 28–30 days to mature, psoriatic skin takes only 3–4 days to mature and, instead of shedding off, the cells pile up on the surface of the skin, forming plaques and lesions. The underlying reason may be due to the hyperactivity of T-cells, which end up on the skin and trigger inflammation and keratinocyte overproduction. Although it is not known why this happens, it is known that the end result is a cycle of skin cells growing too fast, dead cell-debris accumulation and resulting inflammation.
Managing the symptoms
Although there is no cure for eczema or psoriasis, there are ways to manage symptoms, and gaining this knowledge will lead to more satisfied and educated clients. Although eczema and psoriasis are clinically distinct from one another, they do share some common features that may be addressed in the treatment room. Both eczema and psoriasis clients have impaired barrier function and increased inflammation, so your goal will be to protect and repair. Remember to always check first with your client’s physician for contraindications to medications and therapies, because some ingredients may counteract each other. For example, salicylic acid may seem a likely choice for exfoliating psoriatic skin, but could, in fact, inactivate a common topical treatment for psoriasis.
Once a full consultation with the client and possibly her physician is completed, proceed with a treatment using minimal products and procedures. A good way to compensate for minimal skin treatment time is to add on stress-relieving techniques, because there is a psychological component to eczema and psoriasis. Complementary therapies, such as aromatherapy, acupressure, reflexology, massage and inhalation techniques can be coupled with skin treatments to lower stress hormones and control inflammation.
Gentle cleansing and exfoliation is crucial to allow the penetration of rich, emollient moisturizers used on dry, sensitive skin. Avoid harsh exfoliants and detergents, and look for ingredients, such as lactic acid. Use anti-inflammatory ingredients, such as red hogweed, ginger, oats and chamomile, coupled with barrier-repairing oils, including evening primrose, borage, argan and sea buckthorn. Finishing a treatment with a physical sunscreen, such as zinc oxide or titanium dioxide will ensure that harmful UV rays do not cause further damage.
Coaching the client on home care is also an integral part of skin health maintenance. Not only will they need to comply with their prescribed skin care regimen; they will also need to have realistic expectations in terms of time, and expect to see the extended benefits of their treatments long after they are performed. Because these are chronic inflammatory skin conditions, these clients can be a valuable business opportunity, with an increased likelihood of return bookings. Both eczema and psoriasis present highly visible symptoms, and because of this, clients are motivated to help skin improve. Skin health management is a top-of-mind priority for this client’s lifestyle, distinguishing your services from occasional treatments. Don’t be afraid to tackle these skin diseases in the treatment room; the reward could be greatly beneficial to you and your clients.
REFERENCES
1. L Maintz and N Novak, Getting more and more complex: the pathophysiology of atopic eczema, Eur J Dermatol, 17 4 267–283 (2007)
2. HW Walling and BL Swick, Update on the management of chronic eczema: new approaches and emerging treatment options, Clinical, Cosmetic and Investigational Dermatology 3 99–117 (2010)
3. AM Bowcock and W Cookson, The genetics of psoriasis, psoriatic arthritis and atopic dermatitis, Human Molecular Genetics 13 R43–R55 (2004)
4. FJ Smith, et al, Loss-of-function mutations in the gene encoding filaggrin cause ichthyosis vulgaris, Nat Genet 38 337–342 (2006)
5. CN Palmer, et al, Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis, Nat Genet 38 441–446 (2006)
6. SJ Brown, et al, Loss-of-function variants in the filaggrin gene are a significant risk factor for peanut allergy, J Allergy Clin Immunol 127 661–667 (2011)
7. www.niams.nih.gov/health_info/atopic_dermatitis/default.asp#b (Accessed May 3, 2012)
8. S Jacob, M Miller and EM Herro, Atopic Dermatitis—A historical review, Skin & Aging 19 (Suppl) 1–11 (2011)
9. A Cowden and A Van Voorhees, Treatment of Psoriasis (1–9), Switzerland, Birkhäuser Verlag (2008)
Claudia C. Aguirre, PhD is a neuroscientist working as scientific communications manager for The International Dermal Institute (IDI) and Dermalogica. She applies the latest skin-relevant science and technology to the development of curriculum and digital media for IDI and Dermalogica worldwide. Aguirre has received numerous awards, scholarships and fellowships during her studies, and has been published in international scientific journals. She is a frequent editorial contributor to both trade and consumer publications worldwide.